By Dr. Kevin Williams (Chief Medical Officer, Pfizer Rare Disease Unit)
This article is the second installment in the “Ask Dr. Kevin” series, brought to you by Pfizer Rare Disease in collaboration with the National Newspaper Publishers Association (NNPA) to increase understanding of sickle cell disease.
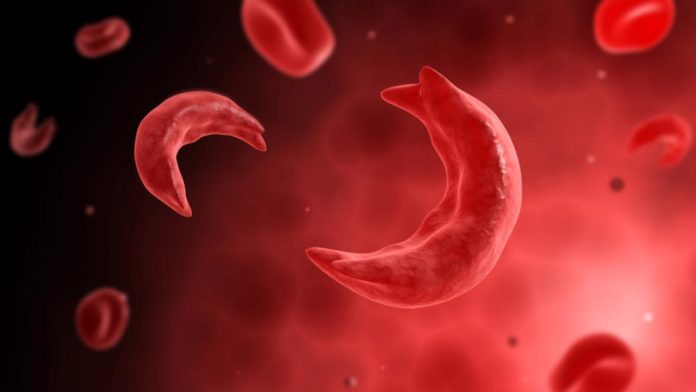
In the United States, sickle cell disease (SCD) is considered rare because it affects only about 100,000 people nationwide. As such, not many people in the U.S. are aware of what SCD is, or if they are aware, they have limited experience with the disease.
As with any disease, low awareness can spur myths and misperceptions and make it more difficult for those affected to obtain the care and support they need. Throughout my career, I’ve been asked a number of questions about SCD—many of which are common myths.
In this article, I will share some of the more common myths, in an effort to separate out the facts from fiction.
Sickle cell disease is a “Black” disease.
Myth! It’s true that in the U.S. more than 90 percent of people living with SCD are of African descent. In fact, SCD occurs in one out of every 365 African American births. However, it’s not exclusive to this patient population. SCD is also found in people of Indian, Middle Eastern, Hispanic, and Mediterranean ethnicities.
Sickle cell disease is contagious.
Myth! You cannot “catch” SCD—it is a genetically inherited condition (passed down from parent to child). For a child to inherit SCD, both parents must carry the sickle cell trait (or have the disease) and each must pass the sickle cell gene to the child.
A person with the sickle cell trait will automatically develop sickle cell disease.
Myth! Sickle cell trait is different from SCD. Just because a person carries the sickle cell trait does not mean they will have the disease. What’s the difference? When a person has only one copy of the sickle cell gene, he or she will have sickle cell trait. Someone with SCD will have two copies of the sickle cell gene.
A person with sickle cell trait can, however, pass the disease on to his or her child, if the other parent also has trait.5 That’s why testing for sickle cell trait or disease is incredibly important. Sickle cell disease (and sickle cell trait) can be diagnosed through a simple blood test.5 In developed countries, like the U.S., babies are now routinely screened at birth to determine if they carry the trait or have the disease.
People with sickle cell disease abuse pain medication.
Myth! Studies have shown that there is no increased substance abuse in patients with SCD. The most common symptom of SCD is excruciating, debilitating pain that often does not respond to over-the-counter medications and needs opioids to provide relief. Over time, the body becomes used to the opioids—ultimately leading to high doses being required to manage SCD pain. This need for high doses of opioids (which may not even provide complete relief from the pain), has unfortunately led to the perception that these patients are “drug-seeking.”
A baby born with SCD will die before reaching adulthood.
Myth! Until the 1990s, SCD was considered a life-threatening condition as many children born with the disease did not live to adulthood. In developed countries, like the US, this is no longer true, with the majority of children living to adulthood, thanks to advances in SCD care.
However, the life expectancy of someone with SCD in the US is only between 40 and 60 years, compared to average US life expectancy of 78.74 years. There is still much more work to do to improve the outcomes of people with SCD in the US and worldwide, particularly in underdeveloped countries. Although the disease was identified more than 100 years ago, there are still very few medicines available to help patients or address SCD symptoms. While there has been recent progress in this area, more still needs to be done. At Pfizer Rare Disease, we are working tirelessly to bring safe, effective treatment options to those in need.
One way to help address this is to encourage participation in clinical trials. To date, there have been several challenges in securing adequate participation of African Americans in clinical trials, which has been one of the key barriers to the development of new SCD medications.
Addressing barriers in clinical trial participation has been a big focus of Pfizer Rare Disease, and working with organizations like the NNPA has been critical in helping spur engagement and action. As part of our collaboration with NNPA, we have sponsored a national poll among the African American community to better understand their perceptions about SCD and participation in clinical trials, and will look to these findings to guide future efforts in this area.
Hopefully, this article has helped to clear up some of the more common misperceptions about SCD. By increasing awareness and providing education about this disease, we aim to improve the care of those affected. Stay tuned for my next article that will discuss clinical trials in more depth and their role in helping to develop potential new SCD treatments.
The next “Ask Dr. Kevin” article will run in December. Meanwhile, here are resources to find more information about sickle cell disease, the collaboration between the NNPA and Pfizer Rare Disease, and a new nationwide poll conducted by Howard University to deepen understanding and gauge perceptions around SCD and clinical trials among African Americans.
Dr. Kevin Williams is the Chief Medical Officer for Rare Disease at Pfizer. He pursued medicine after being inspired by his father’s work as a general practitioner in his hometown of Baton Rouge, Louisiana. Dr. Kevin is passionate about raising awareness and increasing understanding of sickle cell disease in the African American community. You can follow Pfizer on Facebook and Twitter.